[-]
Congenital obstruction of the lacrimal system is present in 1- 6% of newborn children.
Spontaneous resolution happens in 90-95% of cases during the first year of life. In the remaining 5-10% of children, 60% resolve spontaneously during the second year of life. After the fifth year, the probability of spontaneous resolution is minimal. The symptoms of the obstructed flow of tears are: tearing (epiphora), stickiness of the eyelashes due to mucopurulent discharge, and irritation of the periocular skin.
Bearing in mind the statistical data, surgical intervention is thus deferred at least until the 10-th month of life. In the meantime, cleansing of the eyelids should be performed using cotton buds moistened with physiological saline. Massage of the tear sac (lacrimal sac) is done with the small finger. The cleansed eyelid skin should be protected by a thin layer of vaseline (petrolatum gel).
Infrequently, acute inflammation of the lacrimal sac can develop, which necessitates the use of systemic antibiotics.
 Congenital obstruction of the left tear duct (nasolacrimal canal) in a 12 month old infant. The tears in both eyes have been dyed yellow (fluorescein).
Congenital obstruction of the left tear duct (nasolacrimal canal) in a 12 month old infant. The tears in both eyes have been dyed yellow (fluorescein). Acute inflammation of the lacrimal sac in a newborn
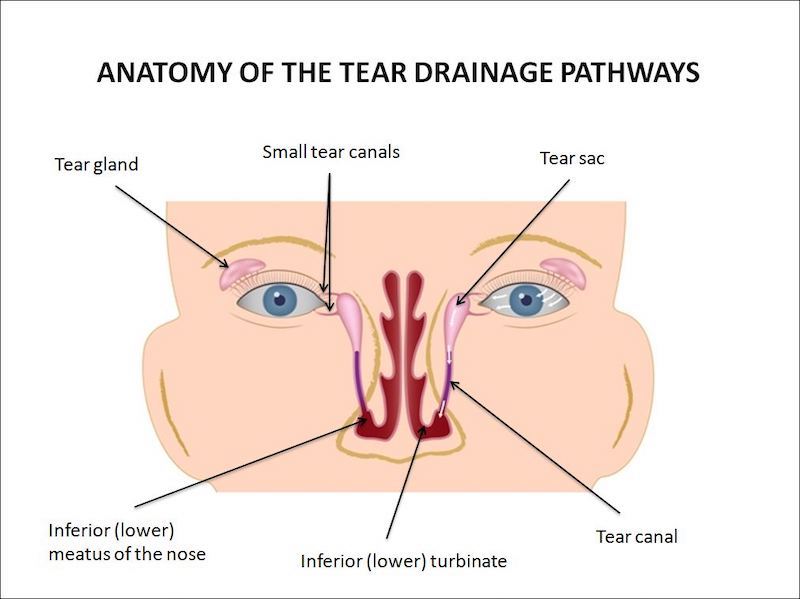
Acute inflammation of the lacrimal sac in a newbornThe surgical intervention, in infants, is performed with a short general anesthesia, allowing the surgeon 10-15 minutes to perform the procedure properly, under controlled conditions, with minimal trauma. The technique involves probing (passing a fine blunt instrument) of the small canals (canaliculi), the tear sac and the tear duct, in order to assess the level and severity of the obstruction. In most cases the obstruction of the tear duct can be penetrated, establishing patency. This has to be done very gently, avoiding damage to these very delicate structures. After this, the system is irrigated with a fine blunt needle, to verify patency and to flush out the accumulated debris.
During the procedure, nasal endoscopy is used to see if there are any other obstructions to tear flow into the nose, such as an enlarged or impacted lower turbinate. If this is the case, the surgeon may need to push the turbinate slightly, away from the opening of the canal.
The last and very important step is the insertion of a silicone stent, the role of which is to maintain patency of the operated tear duct. This is especially important in infants, in whom throat and nose infections are frequent. The atent is removed in the office, after 3 months, and anesthesia is not required for this procedure.
In a small percentage of children, the patency of the tear drainage pathways cannot be achieved with the previously described methods, which is why an alternative path for tears into the nose has to be created surgically by an operation called dacryocystorhinostomy or DCR.
Why is general anesthesia necessary in infants?
Performing this procedure without anesthesia (local anesthesia is not effective in infants) is not recommended due to psycho-physical trauma induced on the child, combined with an increased risk of operative complications due to damage of the delicate lacrimal structures during sudden movements of the head and / or squeezing of the eyelids. Because of crying and irregular breathing, there is a risk of the irrigating fluid being aspirated (inhaled) by the child.
Acquired obstruction of the lacrimal system can occur at any age, but is more frequent in women and middle age. The initial symptoms are only tearing, however, with time, an infection of the lacrimal sac usually develops.
 Chronic inflammation and enlargement of the lacrimal sac
Chronic inflammation and enlargement of the lacrimal sac Acquired obstruction of the tear duct (nasolacrimal canal). Irrigation of the tear duct (painless diagnostic procedure), causes the reflux of mucopurulent discharge accumulated in the tear sac.
Acquired obstruction of the tear duct (nasolacrimal canal). Irrigation of the tear duct (painless diagnostic procedure), causes the reflux of mucopurulent discharge accumulated in the tear sac.Modern surgery of the tear duct is performed without a skin incision, through the nose, with the aid of a special endoscope. The procedure is performed in general anesthesia. A "new tear duct" is created, through which tears will flow into the nose. At the same time, a silicone stent is inserted, which will aid the healing process of the newly formed anastomosis. Recovery after this operation is very quick, as is the return to normal daily activities. The silicone stent is removed in the office, 2 weeks to 1 month after the operation.
The "classic" operation of the tear duct is performed via a skin incision approach – external DCR. The operation can be performed in either general or local anesthesia. The scar at the incision site on the side of the nose is barely visible after 2-3 months. During surgery, a silicone stent is inserted into the newly made opening into the nose, and it is usually removed, in the office, after 1 month. Proper rinsing of the nose at home, combined with endoscopic follow-ups after surgery, is very important in maintaining the patency of the new opening.
The operation of the tear duct can also be performed without a skin incision, with the help of a laser, which is introduced through the small tear canals (canaliculi) into the tear sac. From here, the laser makes a new opening for the drainage of tears into the nose (trans-canalicular laser DCR). It is essential to monitor the effect of the laser, during surgery, with an endoscope inside the nose. The opening created by the laser is smaller in size, compared to the previously described methods, and consequently the success rate is somewhat lower.
In situations where the small lacrimal canals (canalicular system) are completely obstructed, the only solution is to implant a special glass tube, which conducts the tear flow from the inner angle of the eye into the nose: conjunctival DCR and Lester Jones tube insertion.